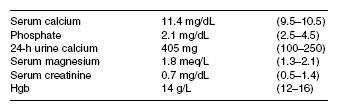
A 58-year-old woman is concerned about her risk for osteoporosis and is seen by her general internist. Her mother was diagnosed with osteoporosis and had a hip fracture at age 84. She has no personal or family history of kidney stones or ulcer disease, and she has never had a fracture. She had a hysterectomy at age 48 and took estradiol for 2 years, but discontinued because of a fear of adverse effects. She does not have any vasomotor symptoms. She takes 1500 mg of calcium carbonate and 400 IU vitamin D daily. She is not on any other medications. On examination, she appears well developed and there is no evidence of kyphosis. ABMD test is performed that demonstrates a T score in the spine of 3.5 and in the hip of 2.8. CXR and mammogram are normal. Further evaluation demonstrates the following:
Which of the following is the most likely diagnosis?
- milk-alkali syndrome
- primary hyperparathyroidism
- sarcoidosis
- secondary hyperparathyroidism
- osteomalacia
Answer(s): B
Explanation:
Primary hyperparathyroidism is common in postmenopausal women and more than 80% present without any symptoms. The most common findings are bone loss, usually in association with estrogen deficiency. The elevated calcium, decreased phosphate, and increased urinary calcium are typical of this disorder. Milk-alkali syndrome is primarily historical disease occurring in patients receiving large quantities of calcium and alkali, and presenting with renal insufficiency, elevated phosphate, and alkalosis. Her normal renal function and relatively low dose of calcium exclude this entity. Familial hypocalciuric hypercalcemia is autosomal dominant and is diagnosed by a low urinary calcium clearance. The lack of renal insufficiency excludes secondary hyperparathyroidism. The normal CXR and Hgb make sarcoidosis and multiple myeloma unlikely. Postmenopausal osteoporosis and osteomalacia are excluded by the elevated calcium level.