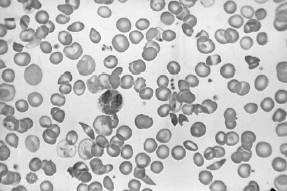
A 23-year-old African-American presents with acute-onset pain in the abdomen, back, and legs. On physical examination, his pulse is 115 bpm, respiratory rate is 20, blood pressure is 100/70 mmHg, and temperature is 101°F. There is scleral icterus, a s ystolic ejection murmur at the right upper sternal border, bilateral rhonchi, a right upper quadrant abdominal scar from a cholecystectomy, and a diffusely tender abdomen without rebound. A neurologic examination is normal. A peripheral blood smear is shown in Figure
.
A CBC with differential and platelets later shows the Hgb to be 6.4, white blood count is 2100 with 85% polymorphonuclear forms, platelet count is 100, and the reticulocyte countis 0.5. Which of the following would be an appropriate next test?
- serum antibody to parvovirus B19
- broad-spectrum antibiotics for sepsis
- consideration for splenectomy
- a bone marrow biopsy
- administration of granulocyte colonystimulating factor (GnCSF)
Answer(s): A
Explanation:
This patient has sickle cell anemia. This is evident from sickle cells forms on the peripheral blood smear in Figure 1-13. Pain medication is an important initial concern. It is often difficult to determine whether a patient in sickle cell crisis has an ongoing infection. Infections can precipitate sickle cell crisis. With respect to community-acquired pneumonia, the diagnosis is difficult. A patient with sickle cell crisis can have fever as a result of the sickle crisis. They can have an increased respiratory rate, physical examination, and CXR findings which suggest pneumonia as a result of pulmonary infarctions. A white blood count can be elevated due to marrow stimulation. In the presence of the acute chest syndrome, characterized by chest pain, hypoxia, and CXR infiltrates, antibiotics would be indicated. Without further information, it is hard to decide to empirically start broad-spectrum antibiotics for community-acquired pneumonia. Transfusions should generally be avoided in patients with sickle cell anemia who are not symptomatic due to the anemia. Since patients in sickle cell crisis have intravascular hemolysis, their reticulocyte counts are usually high and they can replace their blood quickly. Repeated small transfusions will lead to autoantibodies that will make further transfusions difficult. Arterial blood gas determination should not be the first step, given the above information. A CT scan of the abdomen is not indicated given the nonspecific nature of the patient's abdominal findings. Parvovirus B19 can cause aplastic crisis in patients with hemoglobinopathies, including sickle cell disease. A tip to this diagnosis is the decreased reticulocyte count in a patient who normally would have a high reticulocyte count. Given the information listed above, there is no indication for broad- spectrum antibiotics. Splenectomy is not a reasonable alternative at this point. Patients with sickle cell disease have autosplenectomy by the time they are adults. A bone marrow biopsy maybe indicated because of the low platelet count, but not initially. GnCSF is not indicated because the patient does not have neutropenia.
Patients with sickle cell disease typically have isosthenuria.
This is due to repeated infarction of the renal papilli. This causes destruction and interference with the counter current mechanism that causes urine concentration. As a result, patients with sickle cell anemia have the inability to concentrate their urine. This results in fluid and electrolyte abnormalities. Patients in sickle cell crisis are usually fluid depleted. This and the sickled blood cells cause hyperviscosity and microinfarctions. There is no evidence that the patient has diabetes insipidus, which usually has a urine specific gravity less than 1.005. Patients with UTIs do not have isosthenuria due to RBCs and WBCs that increase the urine specific gravity. Sickle cell patients may have zinc deficiency, but this is not a cause of isosthenuria.